Medical billing is a fundamental component of the healthcare system, ensuring proper payment and reimbursement for healthcare services provided to patients. It involves various processes, roles, and types of billing that contribute to the efficient financial management of healthcare organizations. In this article, we will delve into the intricacies of medical billing, exploring its definition, types, processes, and the key roles involved.
What is Medical Billing?
Definition: Medical billing refers to the process of submitting and managing healthcare claims for reimbursement from insurance companies or government programs.
Purpose: The primary goal of medical billing is to accurately record, code, and submit claims to receive rightful payment for healthcare services rendered to patients.
Types of Medical Billing:
Medical billing broadly classified into two types.
Professional Billing: Involves billing for services provided by individual healthcare professionals, such as physicians, surgeons, or therapists.Facility Billing: Pertains to billing for services rendered by healthcare facilities, including hospitals, clinics, and outpatient centers.
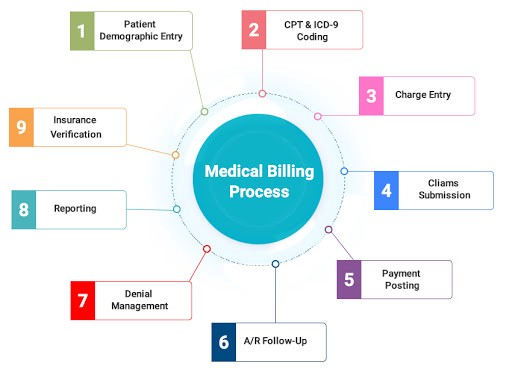
Medical Billing Process:
- Patient Registration: Gathering patient demographic and insurance information.
- Coding: Assigning specific medical codes to procedures, diagnoses, and services using standard coding systems (e.g., ICD-10, CPT).
- Claim Generation: Creating and compiling all necessary information to generate accurate and detailed claims.
- Claim Submission: Transmitting claims electronically or via paper to insurance companies or government programs.
- Adjudication: The evaluation and processing of claims by payers to determine reimbursement eligibility.
- A/R follow-up: Involves actively pursuing unpaid or underpaid claims, resolving billing issues, submitting appeals if necessary, and working towards maximizing revenue collection.
- Payment Posting: Recording and applying payments received from insurance companies or patients to the appropriate accounts.
- Denial Management: Addressing claim denials, identifying reasons, and taking necessary actions to rectify and resubmit claims if needed.
- Patient Billing and Follow-up: Generating patient statements, coordinating with patients for payment, and handling any inquiries or disputes.
Key Roles in Medical Billing:
A. Medical Biller: Responsible for coding, claim submission, and follow-up to ensure timely reimbursement.
B. Medical Coder: Skilled in assigning accurate medical codes to diagnoses, procedures, and services.
C. Claims Processor: Works on behalf of insurance companies to evaluate and process claims.
D. Revenue Cycle Manager: Oversees the entire medical billing process, ensuring efficiency and optimizing revenue generation.
Conclusion:
Medical billing plays a vital role in the financial operations of healthcare organizations. Understanding the various types, processes, and roles involved in medical billing is crucial for healthcare professionals, administrators, and patients to ensure accurate reimbursement and efficient revenue cycle management. By comprehending the nuances of medical billing, stakeholders can contribute to a streamlined and effective healthcare system.

